Is Unmedicated Birth Worth it?: Epidurals & Birth
What a loaded question. But one I still get asked frequently. The answer is entirely dependent on the person asking and how their birth unfolds.
This will end up being a two part blog due to the overload of info in answer to this question.
Let me be clear, I absolutely believe in every woman’s ability to give birth unmedicated, while also acknowledging that isn’t the right choice for everyone or every birth. So, go into this knowing this a judgement free zone and only you can make the right choice for yourself.
Why would someone want to go unmedicated? You don’t get a trophy.
Ok, yes, you don’t get a trophy. But I don’t love that sentiment. Maybe a person just wants to feel empowered by having the experience of a natural, uninhibited birth. It’s never been about trophies, so I cringe when I hear this.
We all love our children no matter how they are born. However, there is something about heading into your birth with the understanding of why doing it without an epidural can be beneficial for both mother and baby; it’s different going into birth without being terrified of labor.
Mindset plays a huge role in how a birth can unfold.
Completing a comprehensive childbirth education class outside of the hospital can really help to prepare you and your partner for the birth. Having a great doula goes a long way, but practicing your mindset and relaxation techniques will go miles for the birth you want in addition to getting a good doula.
An amazing study was done in 2023 called “The mindset of birth predicts birth outcomes: Evidence from a prospective longitudinal study” where doctors studied two different groups of women- those who had a more medicalized view of birth and those who had a more natural view of birth (those are their words, see the study to learn more). I’ll quote directly here so you get the info straight from the horse’s mouth:
Predictions: Conceivably, the mindset and its associated cognitions and emotions could influence the course of the birth, for example, in the sense of a self-fulfilling prophecy. Thus, a more medical mindset could cause the women to be tense during labour, implicitly expecting things to go wrong. Such tension could interfere with the natural hormone release, increasing the probability of complications that then need to be solved with interventions such as episiotomy, vaginal assisted birth, or unplanned/emergency C-section.
Results: The results revealed that the birth-related mindset assessed during pregnancy predicted labour and birth: Women with a more natural mindset had a higher probability of having a low-intervention birth. This in turn had a positive effect on the birth experience, which led to greater general emotional, and physical well-being in the first 6 weeks after birth. Breastfeeding and the well-being and (perceived) behaviour of the infant were also positively affected. These short-term positive effects in turn predicted longer-term psychological well-being up to 6 months after the birth, operationalized as postpartum depression, post-traumatic stress symptoms, and bonding with the infant. These results are crucial as depression in mothers does affect both mother and child, for example, the mother's caregiving ability (Priel et al., 2019) and children's stress response and physical health such as the function of the immune system (Dekel, S. et al 2023).
Mindset matters. So, your job as a pregnant person is to learn about what’s within your power. You can’t control when labor happens or how it unfolds, but you can have some control over your mindset and how you use your toolbox to relax and reset throughout the process.
Is unmedicated birth “worth it”? What are the benefits of Unmedicated Birth?
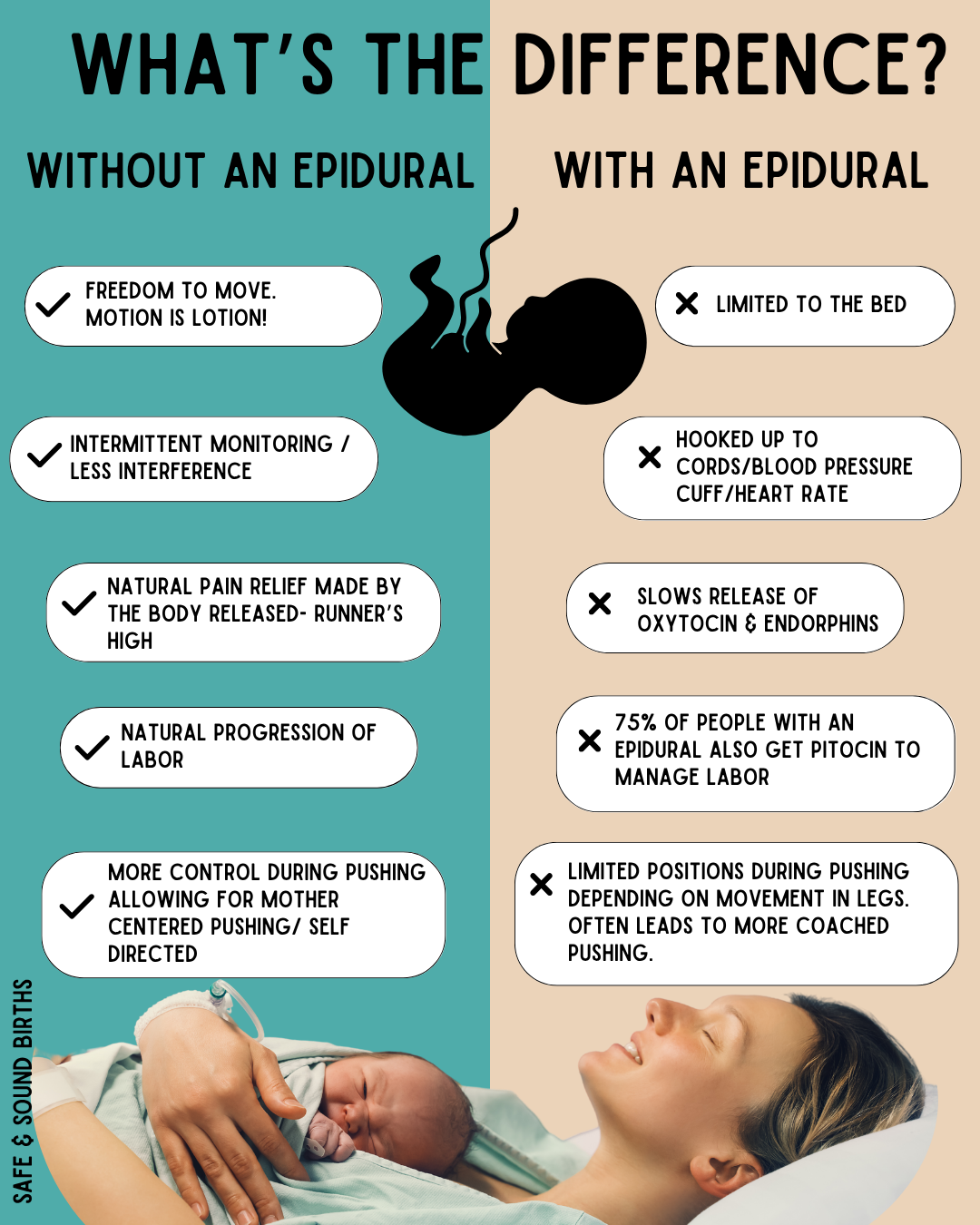
As a teen, I did not see the appeal or understand why anyone wouldn’t want an epidural during birth. I knew nothing about birth other than what was shown in movies and tv shows (which is all terrible information and not at all realistic). The truth is, birth doesn’t have to be terrible. It doesn’t have to be this chaotic thing with you screaming, the birthing team yelling when to push, everything feeling like it’s horrible until it’s over. It can be a beautiful, joyful, calm, empowered experience. You can have that kind of birth with an epidural too. But unmedicated births mean you have more freedom to move around, more say in how your baby is monitored, more agency for how you push (since you won’t be numb in your legs) and much more. The hormonal difference between medicated vs unmedicated is also a big factor throughout the birth.
No matter how you birth, plan on it being the hardest thing you’ve ever done. It will take all of yourself to get through that labyrinth of birth.
Before I can talk about the benefits of unmedicated birth, let’s look at what an epidural actually does.
Monitoring & movement
You don’t necessarily need an IV port in your hand; you don’t necessarily need constant fetal monitoring. These two things are standard when you have a hospital birth, but you can tell them you do not want them. If you have a high risk pregnancy, you’ll need to be monitored more closely. But if you are having a healthy, normal pregnancy, ask if there is any medical indication that you need an IV port and/or constant fetal monitoring. If the answer is no, than advocate for yourself and ask for more freedom.
Let’s talk about TOCO
A toco stands for “tocodynamometer.” It’s a device used to monitor uterine contractions during labor.
Image: Pulling Curls
So, they are monitoring both your baby’s heart rate and your contractions.
Different hospitals have different availabilities with wireless monitors. AAMC in particular is very bad with their wireless monitors. I’ve have good luck at BWMC and Howard County General. But if you have to have constant monitoring, wireless monitors are much nicer.
Image: SGMC.org
If you have to have the belts: The monitor cords are about 6 feet in length, which means you’ll be near or on the bed for most of the labor if you need constant monitoring. This limits your access to different positions you may want to try both because you’ll need to be near the monitor (so things like leaning against a wall or walking around the hallway may be out of reach). Sometimes, when you’re on hands and knees or a forward leaning position, the monitor doesn’t always pick up contractions or baby’s heartrate as well, which means your nurse will be coming in to adjust it and may not be too happy if you continue getting into positions that move the monitor off your stomach (most nurses are wonderful and will help you, but if they’re busy with other patients, another nurse may need to come in).
It also means you can’t utilize the dilation station—laboring on the toilet; or use hydrotherapy such as the bath or the shower to cope with the intensity of the contractions. The toilet is an ideal place to labor because that is where women naturally relax their pelvic floors. It can make contractions more intense, but that is a good thing. We need to get that baby putting pressure on that cervix to help bring your baby here.
What’s more, the bathroom (esp at the hospital) is a much more private situation than the open room with the bed. You can really adjust the lights in there by bringing your own (or using my fairy lights) and have this intimate, private space to truly relax into the sensations of labor. Privacy helps women to feel less watched, more relaxed, and feel safer overall—all of which help to release oxytocin to help bring your baby here.
Details of the Epidural
If you have an epidural, you might have pretty good use of your legs. I have been to a number of births at different hospitals where women have full, working epidurals and are still able to get themselves into the hands and knees position to push their baby Earthside. However, some women are very numb and their legs feel very heavy. This not only makes it difficult to move during labor, but it also makes it hard to feel if you’re pushing the right way. A mirror can be a big help in making that mind-body connection if you’re able to watch yourself pushing and see yourself making progress.
It feels strange to push when you can’t tell if you’re having contractions (so you’ll need to be on the monitor and they’ll tell you when you’re having one by watching the screen) and it means you’ll need a lot of coached pushing. This can be appropriate for some people. But if you’re more inclined to have a more relaxed , self guided approach to pushing, this can feel very overwhelming. I have heard providers say “Get mad at your baby! Get mad and push them out!!” which, I know that would work as motivation for some women, but most of my clients are looking for a loving, gentle approach to their births. Getting mad at their baby to push seems really counterintuitive to that. Providers will (mostly) listen to your feedback if you tell them what you’d like. But you’ve (hopefully) met these people- some doctors are warm fuzzies, some just aren’t. That doesn’t mean they’re not good at their job—they just have a different approach than maybe the one you’d want. And I’ll tell ya, whatever doctor you don’t want will probably be the one on-call when you go into labor HAH! You can always ask for another doctor, but sometimes the devil you know vs the one you don’t is the better option.
You can absolutely still move from side to side with a very numbing epidural (with the help of your birth team—I don’t want you to think you have to push on your back!) and you are able to ask the anesthesiologist to turn the epidural down so you can have more sensation. This sometimes works, but not always. When you get an epidural, the anesthesiologist usually asks for your height, weight, and history of anesthesia. Some ask about if you have scoliosis, but not always (do mention it if you have it!). The medication amount they give you is based on height and weight. If you know you react strongly to medication, tell the anesthesiologist this.
Anne Arundle Medical Center allows partners and doulas in the room for the epidurals. University of Maryland Baltimore Washing Medical Center (BWMC) does not let anyone in the room for epidurals. They claim it is to keep the room sterile. This is a weak claim being that other hospitals don’t have this policy and if it were really dangerous, AAMC wouldn’t do it. So, if you’re birthing at BWMC, just know you’ll get the epidural by yourself because they kick everyone out. I hate this policy for a number of reasons.
Either way, once you get an epidural (whether or not you can move your legs around), the policy is for you to stay in bed. We can put you in different positions to help bring baby down, but being able to stand up, sway & dance have waved bye-bye once you have an epidural. Which is still sometimes the right choice, but I’m just informing you of all the angles involved with an epidural.
When you get one, you are at risk for low blood pressure by the very nature of the medication they give you. So, once you want one, you’ll tell your nurse. They will then need to give you a bag a fluids to help with the risk of low blood pressure. Many women get dehydrated during labor. To prevent this, your partner should be offering you water regularly. Enough to make you need to pee hourly.
I tell all my clients that their partners are their own personal waterboys (or watergirls). When you’re dehydrated, your risk of low blood pressure goes up with the epidural, so that’s why they need to give you the saline solution. This usually takes about 20-25 minutes. Once the anesthesiologist comes in, it can take anywhere from 10-20 minutes to get the medication in place. If you’re having contractions 4 minutes apart at this time, it means you are going to have contractions while you’re getting this medication placed in your lower back and you must remain still, and curled around your baby.
Howard County General Hospital has these amazing epidural chairs that look like those massage chairs at the mall. You don’t have to just curl around your baby—you can settle down into those chairs. But if you’re not birthing there, you’ll have to shrimp yourself into this position.
Image: SPHP.com
Past client getting ready for her epidural.
Image: My Health Alberta, CA.
Once the medicine is in, it can take about 20 minutes to feel the full effect. It is not a BAM! pain vanished kind of thing. It usually goes away slowly—most people feel like the contractions get shorter and shorter until they cannot feel them any longer. Then you can hopefully take a nap and we’ll move you around using the peanut ball based on what station your baby is in your pelvis.
However, for the first bit of time, you will have your blood pressure cuff going off. It is loud and tight and most people hate it. It varies from every three minutes immediately following the procedure, to the standard I see most often, which is either every 15 minutes or every half an hour until the baby is born. It does this while you’re sleeping, sometimes while you’re having contractions. It does not care what you are doing—it goes off on a timer.
Some people can sleep through this (especially if you’re tired enough), but not everyone can. Alarms are constantly going off in the room and unfortunately, most nurses get what is called ‘alarm fatigue’ where they don’t even hear them anymore. You can hit the ‘silence alarm’ button, but it’s only silenced for 2 minutes. They’re taking your blood pressure, but also your pulse and oxygen levels will be monitored. So you’ll have on a little sticky wire on your finger (or sometimes they’ll put it on a toe).
Image: Linked In.
Quick Note On Movement- Movement is what can help get your baby out. You can still move with an epidural, but being in a bed does limit your movement. With unmedicated pushing, a woman is better able to feel what she is doing instead of being numb. She’s able to move her body on her own (as opposed to her legs being held up in one place, sometimes at the mercy of what the doctor has to say about moving).
If I’m your doula, I have women move every 5-6 contractions when pushing. Side to side, closed knee pushing, extended side lying, etc. There are options for epidural pushing positions, but only if you know to advocate for yourself if you have a doctor who is not super into changing positions. Some doctors just want you to push on your back because it’s easier for them. It’s easy to just let them take over. And sometimes pushing on your back is the right choice. But my job is to make sure you know your options.
Become like the ocean- flowing and moving; liquid movement of softness and power.
That is one reason why holding off on an epidural until you’re in active labor can be helpful because once you hit 6cm or further along, things tend to progress more quickly than how long early labor tends to move.
Flood of Natural Hormones
An epidural absolutely changes the labor hormones that are released within the body vs birthing without one.
Most people are aware of oxytocin’s involvement in birth. It is called the love drug (not me over here considering an oxytocin molecule tattoo) and it helps bring on labor, helps labor to progress, helps you fall in love with your baby after birth. This is one powerful hormone. Pitocin is the synthetic form of oxytocin, but it is not the same. It is used to either bring on contracts, help contracts get into a better pattern (helping contractions that are 8 minutes apart move down into 4 minutes apart), or can help increase the strength of the contractions.
Additionally, epidurals reduce your body’s production of oxytocin. According to a study released in 2002 (we’ve known this that long!!), epidural “during labor may interfere with the release of plasma oxytocin, which may be one mechanism behind prolongation of labor” (Rahm 2002). It interferes with the love drug that helps bring your baby here! That is why so many women with epidurals end up with Pitocin. 75% of women who get an epidural during labor also receive Pitocin for labor augmentation (Rossen 2018).
An Epidural Blocks that runner’s high
With unmedicated birth, nature’s natural pain relievers are released, making the contractions feel more manageable (although still very intense). It’s the same thing that happens to runners-endorphins are released during natural birth to help combat the (painful) sensations of birth.
BUT I will say,
Giving birth is not like breaking your arm. The contractions are intense—they take all of you to get through them, especially hours into it—but they aren’t an injury. And you’ll be shocked at how much you are in complete concentration during a contraction, breathing through that sensation and then it just goes away once the contraction is over. You get a break. Those times in between contractions are there for you to recover and laugh and move—whatever feels good to you in that moment. I was roaring my baby down trying to get to the car with my second baby and my 19 month old daughter was freaking out. As soon as the contraction was over, I was able to laugh and tell her “oh it’s ok, mama’s just having the baby!” I couldn’t believe how normal I felt in between contractions. Being able to move around helped me so much. Being able to feel when I was having contractions helped tell me I was making progress.
The big take away here is that when you medically manage your labor with an epidural (and for 75% of women, that leads to use of IV Pitocin), the labor cocktail you would naturally produce is not there. An epidural still might be the right choice, but there are pros and cons to both getting an epidural or not getting one.
Recovery
Unmedicated birth recovery is a little different—with my first baby, I had an epidural ten hours into back labor and gave birth 13 hours later. I pushed for four and a half hours and she came out looking right at me, sunnyside up. That is why the pushing took as long as it did and the epidural was the absolute right choice. However, due to how long I pushed—I was grabbing behind my legs and doing about a thousand crunches pushing that baby out and the next day, I felt like I had been in a car wreck. Everything was so sore.
When you get an epidural and anyone helps hold your legs open (whether on your side or on your back), you are numb so you aren’t able to tell us where your stretch limit is if they open your legs wide. Because of this, you’re often extremely sore the next day because we’ve stretched you further than you could have stretched on your own.
I thought that was just how you felt after giving birth. But when my second came in the car and the ambulance showed up seven minutes later, they told me they were going to lift me onto a stretcher and roll me into the ambulance. My daughter was still on my chest, umbilical cord still attached, placenta still waiting to be birthed. I laughed at them saying they’d lift me up and I got up out of the car and walked into the ambulance holding her, cord still hanging out. I felt amazing. And the next day, I didn’t feel sore the same way at all as that first birth. It was such a different experience.
With an epidural, they will turn it off after delivery and you should be able to walk to the bathroom (with the help of the nurses) within two hours of it being off. Because you need the urinary catheter with the epidural (because you can’t get out of bed to pee), it can sometimes take longer for your bladder to remember how to work on its own, but it should return to normal shortly.
In the USA, upwards of 70-75% of women choose to get an epidural when giving birth.
There aren’t studies to say how many of those women had the goal of an unmedicated birth. I can tell you anecdotally from my experience with my clients that probably 50% intend to give birth unmedicated, but 75% end up choosing an epidural. That stat is obviously very different for my home birth clients who don’t have access to an epidural.
This post went over what all an epidural entails. Next week, I will delve into what unmedicated birth can feel like—why people choose to do it beyond the reasons listed above.
With birth, whether medicated or not, your body does know how to do this in the same way it knew how to grow the baby—the same way it knows how to digest food and make your heart beat. It’s innate. So believing in your ability to give birth and your body’s knowledge of how to do it helps everything go more smoothly. A good comprehensive childbirth education also goes far, as well as having a doula on your birth team.
There are good reasons to get an epidural and I stand by my choice to get one with my first baby. There are also lots of reasons to skip it and get your body ready for the demands of labor throughout your pregnancy so you feel prepared for what labor will truly be—a labyrinth of love, pain, sensation, movement, and joy.
Sources
Rahm, V.-A. (2002). Plasma oxytocin levels in women during labor with or without epidural analgesia: A prospective study. Acta Obstetricia et Gynecologica Scandinavica. https://pubmed.ncbi.nlm.nih.gov/12421171/
Rossen, J., Klungsøyr, K., Albrechtsen, S., Løkkegård, E., & Rasmussen, S. (2018). Can oxytocin augmentation modify the risk of epidural ... Acta Obstetricia et Gynecologica Scandinavica. https://obgyn.onlinelibrary.wiley.com/doi/full/10.1111/aogs.13341
G. Carroll, T., Engelken, M., Mosier, M., & Nazir, N. (2003). Epidural analgesia and severe perineal laceration in a ... The Journal of the American Board of Family Medicine. https://www.jabfm.org/content/jabfp/16/1/1.full.pdf